Deadly
microbes that cannot be destroyed invade the human body, mutating and
multiplying at such a rapid rate that the entire global population is
imperiled. Sound like the logline of a sci-fi horror film? It’s
actually a very real synopsis of the impending health apocalypse. The
World Economic Forum’s 2013 Global Risk survey cited antibiotic resistant
bacteria among the top 50 risks threatening the human population.
We’ve been careless with our most valuable weapon:
antibiotics. In less than eighty years after antibiotics were created we
are now suffering the consequence of our abuse.
As more and more strains of antibiotic resistant bacteria
mutate and spread, our ability to fight back diminishes—antibiotics are no
longer the weapons of mass destruction they once were. Our ammunition has
been used up and our battle-axes are now rusty and defunct.
A Brief History of Antibiotics
Scientists
began the quest for antibiotics in the late 1800s as the germ theory of disease
was gaining scientific acceptance. The germ theory linked bacteria and
other microbes with various illnesses, and scientists realized how valuable it
would be to find a chemical substance that could destroy particular pathogens.
It
wasn’t until Sir Alexander Fleming accidentally discovered penicillin in 1928
that the antibiotic solution gathered momentum. The first antibacterial
drug sulfa was developed in 1935, and Nobel Prize winners Howard Florey and
Ernest Gain developed Penicillin G Procaine to be marketed as a drug in 1942.
After
World War II the antibiotic assault was in full gear with
Tetracycline, Amoxicillin and Trimox joined the ranks and cured fatal, and
previously untreatable, infections at the time.
Where We Went Wrong
Antibiotics
don’t launch an attack against a specific infection, but go on an all-out
destruction path to sweep out of trillions of bacteria—both good and bad—in the
body.
Bacteria
are incredibly resilient, however, and the sheer number of bacteria, coupled
with the ability to mutate into ever-resistant strains, gave some bacteria an
advantage. The bacteria that survived doubled their efforts and
multiplied, and won the war against antibiotics.
How did we lose our offensive advantage
against disease?
By over-prescription, coupled with the use of
antibiotics in livestock, this nullified the potency of antibiotic therapy.
Prescription-happy
doctors doled out antibiotics to cure non-infectious ailments such as colds and
viruses that don’t even respond to antibiotic treatments. The more we
exposed bacteria in our bodies to antibiotics, especially when antibiotic
treatments weren’t called for, the more resistant they became.
Perhaps
the biggest culprit is the agricultural industry, which pumps livestock full of
antibiotics in order to fatten up our meat. Europe banned the use of
antibiotics in livestock years ago, but the United States still uses 30
million pounds of antibiotics in livestock each year! Bacteria resistance
accumulates in cattle and is passed down to humans through food.
That’s
four times the amount of antibiotics prescribed by doctors, according to the
United States Food and Drug Administration (FDA).
No Chance of Containment
We
cannot depend on the drug companies to help us. The pharmaceutical
industry doesn’t want to invest hundreds of millions of dollars on an
antibiotic that is only used for short-term benefit.
Drug
companies would rather spend their money developing drugs for chronic
illnesses… drugs that need to be used over a lifetime in order to recoup their
investment.
It’s
shocking to discover that no new antibiotic treatments have been proposed in
over ten years! And it doesn’t look like the government is going to be
much help either. There have been no restrictions placed on the use of
antibiotics to spur livestock growth. It’s up to the individual to
contain the rampant spread of daily antibiotic resistant bacteria.
Arm Yourself with Knowledge
Before antibiotics people fought off infectious diseases
quite effectively with natural remedies, HERBS and
oils, soaps and salves that didn’t harm a single cell in the body. It’s
imperative that we get reacquainted with our natural heritage.
In another article from Nature World News, researchers have uncovered
two cases of U.S. patients infected with bacteria carrying an
antibiotic-resistance gene, a troublesome development in the eyes of scientists
and health care officials. The new findings feed a growing fear that today's
faltering antibiotics will leave even the developed world defenseless against
increasingly resistant "superbugs."
"The
golden age of antibiotics appears to be coming to an end," writes health
reporter Melissa Healy in the L.A. Times.
She cites research showing that 70% of Americans are unaware of the growing
danger posed by highly resistant pathogens. "It's a slow
catastrophe," said Colonel Emil Lesho, director of the Multidrug-resistant
Organism Repository and Surveillance Network (MRSN), to Healy.
When the British biologist Alexander Fleming
discovered penicillin in 1928, he ushered in an age of modern medicine equipped
with the "wonder drugs" it needed to fight the spread of many
bacteria-borne illnesses, including tuberculosis, syphilis, diphtheria and even
leprosy. But it was not long after the advent of mass-produced antibiotic
agents that medical workers began to encounter drug-resistant strains of bacteria.
Over time, more and more antibiotic medicines
have lost their "wonder drug" status as an increasing number of
resistant "superbugs" has emerged. But health workers have always
been able to rely on colistin - a medicine that is toxic to the human kidney,
but nevertheless the avenue of last hope to many a desparate patient.
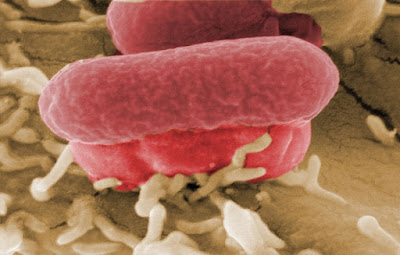
Now, that hope is dying. On May 18, MSRN
scientists at the Walter Reed Army Institute of Research analyzed a sample of
E. coli bacterium taken from a Pennsylvanian woman and found that its DNA
possessed the mcr-1 gene, which makes the microbe untreatable with colistin.
On July 11, JMI Laboratories researchers
published a study that
revealed a second U.S. case of infection by an E. coli bacterium carrying the
mcr-1 gene. The "superbug" was detected in a year-old sample from a
patient in New York.
Science Daily reports
that the lab team is investigating whether the mcr-1 gene discovered might be
plasmid-mediated, a serious concern because "plasmids, genetic elements
that are independent of the host genome, often jump between different bacterial
species, spreading any resistance genes they carry."
The Antibiotic Apocalypse Explained


No comments:
Post a Comment